CanadaWaits.ca
Important health care statistics and solutions. One location.
Canadians Waiting for Health Care:

How many Canadians are waiting for surgery, to receive a diagnostic scan or see a specialist?
Below are the figures provided to SecondStreet.org by provincial governments across Canada.
Click on each province’s name to see our data source.
|
Province |
Surgery |
Specialist |
Diagnostic |
Percent of population waiting for surgery** |
Date |
|
96,076 |
– |
242,902 |
1.7% |
April 15, 2025 |
|
|
Alberta |
1.6% |
April/July, 2025 |
|||
|
31,902 |
– |
2.5% |
June 30, 2025 |
||
|
10,635 |
– |
88,944 |
0.7%* |
June, 2025 |
|
|
233,679 |
– |
719,710 |
1.4% |
December 1, 2024 |
|
|
151,355 |
908,689 |
450,544 |
1.7% |
Feb/March, 2024 |
|
|
New Brunswick |
– |
2.7% |
Mar 31/June 30, 2025 |
||
|
18,237 |
– |
43,197 |
3.3% |
March 31, 2025 |
|
|
15,453 |
23,469 |
95,663 |
1.4% |
May 1, 2025 |
|
|
– |
– |
– |
– |
April 15, 2025 |
|
|
‒ |
‒ |
‒ |
‒ |
June 3, 2025 |
|
|
1,311 |
14,738 |
2,520 |
2.9% |
Aug/Sept, 2025 |
|
|
320 |
2,457 |
7 |
0.8% |
April 22-25, 2025 |
|
|
TOTALS: |
664,338 |
1,205,370 |
1,902,714 |
|
|
|
|
|
Grand Total: |
3,772,422 |
* Only includes surgical figures for cardiac, cataract, knee and hip operations, so this figure is likely thousands below the true total.
***The specialist data provided by Nova Scotia only counted waitlists for a few types of specialists. As such, the numbers are likely much higher. In addition, the province has not provided new diagnostic waitlist numbers since June 2022.
As you can see, several provinces didn’t provide complete data.
Using cautious assumptions, and the data available, we estimate if those blanks were filled in, the true total number of Canadians waiting for health services is closer to 5.8 million.
We came to that conclusion using these assumptions:
Prince Edward Island – Using data from the three other Atlantic Provinces, we calculated there would be approximately 4,144 patients waiting for surgery and 14,810 waiting for a diagnostic scan.
Appointments with Specialists – Quebec, Alberta, Nova Scotia, the Northwest Territories, and Nunavut were the only jurisdictions to provide SecondStreet.org with estimates on the number of patients waiting to meet with a specialist. We combined the data from those jurisdictions, and compared the number of patients on a waitlist to the total population of those provinces. That gave us a rate of over 7.9% of the population on a waitlist to see a specialist. Applying that 7.9% number to the other six provinces gives us a total of 2,056,288 patients waiting to see a specialist in those provinces.
Wait Times in Canada:
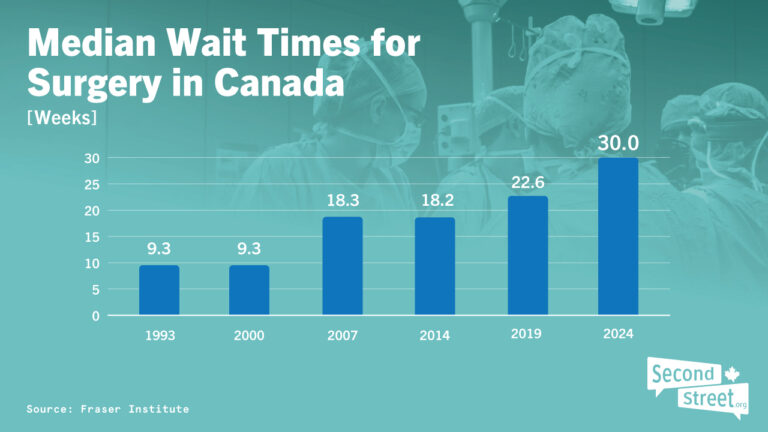
Since 1993, the Fraser Institute has been conducting extremely valuable research on the amount of time Canadians spend on waiting lists.
As you can see in the infographic above, a patient’s typical wait from referral to a specialist until they actually receive surgery has more than doubled. Here are links to the data used in the graphic above:
2024 Waiting list estimate ‒ click here
2023 Waiting list estimate – click here
2022 Waiting list estimate – click here
2021 Waiting list estimate – click here
2019 Waiting list estimate – click here
2014 Waiting list estimate – click here
2007 Waiting list estimate – click here
2000 Waiting list estimate – click here
1993 Waiting list estimate – click here
Patients who are interested in learning more about their province’s waiting lists are encouraged to visit their province’s Department of Health website – some have spent considerable time pulling together the latest data.
Patients Dying on Waiting Lists:
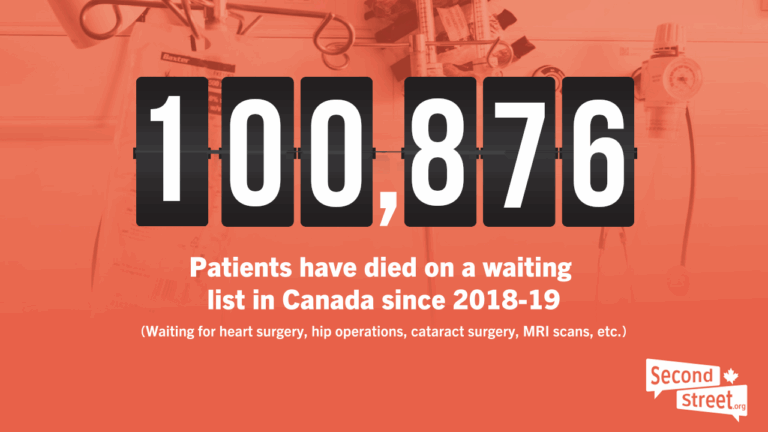
Several stories in the media led SecondStreet.org to investigate how often patients die on waiting lists in Canada.
One of those stories was Laura Hillier’s tragic experience with Ontario’s health care system in 2016.
Hillier was a young 18-year-old girl who died on a waiting list while waiting for a stem cell transplant. A video capturing her desperate cry for help went viral on social media. The teen had a donor lined up and was ready for surgery, but the government hadn’t rationed enough money for hospital beds and staff to treat her, so Laura waited … and waited … before eventually passing away.
Michel Houle, Jerry Dunham and Shannon Anderson are other examples of this serious problem in Canada.
Perhaps what’s just as bad is that many governments don’t even know how often this happens. They simply don’t track the data. Other governments do gather the data – seemingly by accident – but don’t bother to analyze it.
Since 2019, SecondStreet.org has filed information requests with provincial governments across Canada to gather data on the number of surgeries, diagnostic scans and appointments with specialists that have been cancelled as the patient passed away. The data is often incomplete, but it appears that most die while waiting for procedures which would be unlikely to save a patient’s life – a hip operation, cataract surgery, etc. However, these cases cannot be ignored – would you want to spend the final year of your life living with chronic pain? Cloudy vision? Stuck in your home because you felt like you couldn’t go out?
To date, we have identified over 100,876 patients who have died on waiting lists. This does include cases where patients died while waiting for surgeries which could have potentially saved their lives. For instance, in 2022-23, the Nova Scotia Health Authority noted there were 532 patients who died while waiting for surgery and of those 50 died while waiting for a procedure which could have potentially saved their life. Of the 51 cases, 19 died after waiting longer than the recommended wait time. To see this data from the Nova Scotia government – click here.
To view our Died on a Waiting List reports and all our data sources, please see these links:
November 2025 report and news release ‒ click here
July 2025 update from Interior Health (B.C.) ‒ click here
April 2025 update from Quebec ‒ click here
January 2025 report and news release ‒ click here
November 2024 update from New Brunswick ‒ click here
November 2024 update from Saskatchewan ‒ click here
November 2024 update from Ontario ‒ click here
May 2024 update from Saskatchewan and B.C. – click here
2022-23 Report and news release – click here
August 2023 update from Ontario – click here
March 2023 update with Ontario, Alberta and Manitoba data – click here
January 2023 update from Saskatchewan – click here
2021-22 Report and news release – click here
2020-21 Report and news release – click here
2019-20 Report and news release – click here
2018-19 Report and news release – click here
Government Spending on Health Care:
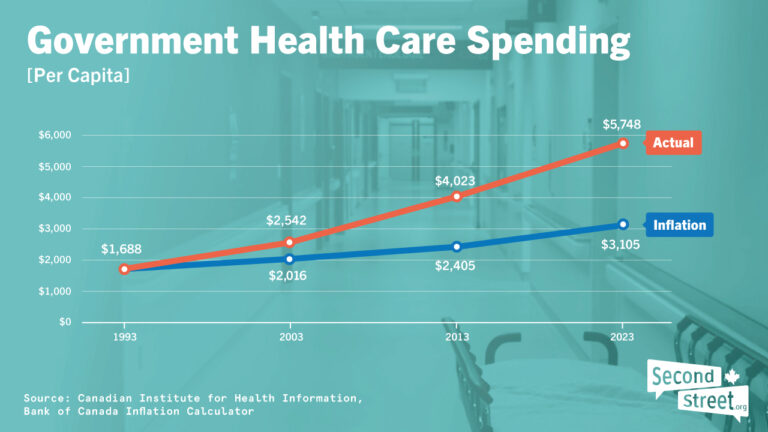
Since 1991, government spending on health care in Canada has increased at more than double the rate of inflation.
While some special interest groups like to talk about “health care cuts,” on the whole, that’s just not true.
The data above comes from the Canadian Institute for Health Information’ (CIHI). They’re a provincially-funded body that gathers all kinds of health care statistics. See “Series F” on this page to download the data and review it for yourself (click on the “Canada” tab and review “per capita” expenditures).
Solutions:
Canada’s health care system is complex and requires many different policy solutions to improve results. In 2024, SecondStreet.org released Health Reform Now, a 40-minute documentary that examines five health care solutions from Europe. Watch it below:
Here is more information on a few important measures that governments could enact to help patients:
1) Track the Data: It’s hard to address a problem in a complex system if you don’t have good data. As noted above, eight provinces couldn’t provide data on the number of patients waiting to see a specialist. Some couldn’t provide data on the number of patients waiting to receive a diagnostic scan or surgery.
Further, SecondStreet.org’s investigation into cases of patients dying on waiting lists has shown that many health bodies in Canada simply don’t track the data (including most of Quebec and Newfoundland) and most don’t even analyze the data they do track.
Thus, a good first step would be to improve the tracking and disclosure of data in the health care system. This would allow policymakers to focus on areas for improvement and be held accountable.
2) Activity-based funding: Instead of provincial governments providing annual cheques to hospitals each year and hoping for the best, studies have shown that hospitals perform better when their funding is based on their output. In short, using an “Activity-based Funding” approach means that every time a hospital completes another knee surgery, it would receive another, say, $5,000.
Suddenly, patients aren’t seen by hospitals as another problem they have to deal with, but rather as a patient they want to deal with as helping them means more funding. This approach requires governments to carefully calculate the cost of a procedure, allowing them to also determine if any non-hospital providers (third parties) are able to provide the procedure.
To read a Fraser Institute report on this option – click here
To read a Montreal Economic Institute report on this option – click here
To watch a short video about this option – click here.
3) Keep the public health care system, but allow patients to pay at private clinics: Prior to COVID, many surgeons would tell you that they had lots of free time. This was due to the fact that the government hadn’t allocated enough funding for them to provide more surgeries. This is an example of what people refer to as “rationed health care.” (This article discusses the “cap” on surgeries in Alberta.)
Something that more successful universal health care systems around the world do is give patients a choice: use the public system or pay out of pocket at private clinics. This helps take pressure off the public system as some patients decide to pay for care rather than wait and depend on the public system.
We talk about this option in this video if you would like to learn more – click here.
4) Copy the EU’s cross border directive: If provincial governments copied a health care policy from Europe, they could immediately help thousands of Canadian patients who are suffering.
Passed in 2011, the European Union’s (EU) “cross border directive” takes power out of health bureaucrats’ hands and instead puts patients in the driver’s seat. EU patients facing a long wait list for a procedure can travel to another EU country, pay for surgery and then be reimbursed by their home country for the bill. Reimbursements cover up to the cost of what the government would have paid to have the procedure done locally.
To understand how it works, imagine Luigi, a fictitious patient in Italy who was told by his government that he would have to wait four months to receive knee replacement surgery. In the meantime, he’s not working, living with chronic pain and taking painkillers. His life is basically on hold.
Instead of spending four months waiting for surgery in Italy, Luigi decides he wants to explore surgery in another country. He then finds a clinic in France that could do the surgery he requires in a couple weeks for $10,000. As luck would have it, his government would normally pay $10,000 to have the surgery done locally. Thus, if Luigi chooses this option, he would pay $10,000 for the surgery and then be reimbursed $10,000 from the Italian government when he returns home. Travel expenses and lodging are his only costs.
To learn more about this policy option – click here.
5) Partner with Private Clinics: Before purchasing a car or home, most people shop around. In health care, governments often choose to deliver services to patients internally, but there are plenty of examples of how hiring private clinics can help patients while reducing costs.
In Saskatchewan, the government faced long waiting lists in the health care system and chose to address this problem by implementing the “Sask Surgical Initiative.” In short, the government hired private clinics to provide surgeries to patients at no charge – just as a patient would receive in a government-run hospital. The clinics had to meet the same standards and deliver the services in a cost-effective manner.
According to research by the Fraser Institute, the government was able to reduce wait times while also reducing costs.
To view the Fraser Institute’s report on this initiative – click here
To view the Sask government’s responses to our questions about this initiative – click here
To view a short video discussion on this initiative – click here
