A Look at the Saskatchewan Surgical Initiative
Can you tell us about what led to the provincial government coming up with the Saskatchewan Surgical Initiative?
In 2008, the Government of Saskatchewan commissioned an independent, first of its kind in Canada, review of the issues and challenges facing the Saskatchewan health care system from the perspective of patients, their family members and advocates. Entitled, “The Patient First Review”, this report’s findings confirmed that surgical wait lists were a primary concern for patients and their families. Work began immediately on a comprehensive and focused reform of how surgical services are coordinated and delivered in Saskatchewan and with the goal of addressing as many bottlenecks as possible.
The Saskatchewan Surgical Initiative was launched in 2010 as the government’s plan to implement the public’s desire to shorten surgical wait times and improve the experience of surgical patients in Saskatchewan.
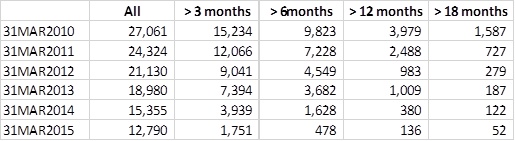
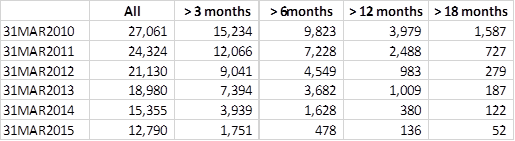
The first year goal of the Saskatchewan Surgical Initiative was to have no patients waiting longer than 18 months for surgery. The system was challenged to meet that goal and a year later, there remained more than seven hundred surgical patients still waiting 18 months for their surgeries.
It was decided that in addition to ramping up surgical capacity in publicly operated facilities, an expansion of publicly funded third-party delivery of selected surgical and diagnostic services should also be added to the Saskatchewan Surgical Initiative to further reduce wait times. Third-party facilities were contracted as a way to increase surgical volumes, without having patients jump the queue or pay for services.
Saskatchewan did hire more staff and increased surgical capacity in (its) publicly operated facilities. The Saskatchewan Surgical Initiative expanded both publicly and privately delivered surgical services to reduce wait times; however, additional capacity was required to address the backlog of those patients waiting longest.
Saskatchewan remains committed to publicly funded, publicly administered health care and maximizing surgical capacity in publicly operated facilities. By contracting third party facilities, this provided additional capacity for the Province to perform more surgeries in addition to those provided in hospital settings.
During the five years of the Surgical Initiative (2010-11 to 2014-15) the Government of Saskatchewan provided a cumulative investment was approximately $235M. The goal of this initiative was to remove bottlenecks in the surgical system and reduce wait times. Potential cost savings were not prioritized for consideration.
Costing comparisons of the original contract awards for third party surgical facilities demonstrated all procedures were performed below the cost of the public system. More recently, comparisons using estimated public system costing for surgeries based on a resource weight methodology developed by the Canadian Institute for Health Information show costs per procedure can vary based on complexity of the patient, we do not calculate actual cost per each procedure performed. Based on this more recent analysis, assessments showed that the difference between per-procedure costs in public hospitals and private surgical centres are roughly 35 per cent in plastic surgery and general surgery day procedures, and up to 45 per cent in orthopedic day procedures. Note that our private surgical partners typically perform less complex surgical cases as they are unable to keep a patient overnight or for an extended recovery, which contributes to some of the cost differences reported here.
You can help us continue to research and tell stories about this issue by making a donation or sharing this content with your friends. Be sure to sign up for our updates too!


