Imagine you just finished waiting six months to finally meet with a specialist about your knee – the situation was so bad that even walking across your living room was a painful ordeal. The specialist reviewed your diagnostic scans, asked you a few questions and then recommended surgery – you’re told the wait time is a year.
This example is far from a fantasy: wait lists are ballooning across Canada, emergency rooms are overwhelmed, and health care costs are climbing. Some patients are even dying while waiting for treatment.
But what if more Canadians never needed treatment in the first place? That’s where preventative health care comes in – and Canada is falling behind.
These staggering statistics characterize Canada right now:
- 30 per cent of adults are considered obese and 37 per cent are physically inactive.
- Only 39 per cent of children get the recommended amount of daily physical activity
- Fewer than 1 per cent of teens meet the full national guidelines for exercise, screen time, and sleep
But it’s not just exercise that Canadians are deficient in – countless stories appear in the news each year that highlight dietary problems in our nation as well. Ultimately, the aforementioned stories aren’t just lifestyle choices. They’re a recipe for expensive, painful and dangerous chronic disease.
The Canadian Cancer Society’s website notes that “about four in ten” cancer cases are preventable. Almost 80 per cent of premature heart disease and stroke can be prevented through healthy behaviours, according to the Heart and Stroke Foundation. This summer I was asked to explore what governments in other countries are doing to promote prevention. It was interesting to see a wide array of approaches – from policies that provide a gentle nudge toward healthier living to policies that are more aggressive (and would never be accepted in Canada). Here are five international prevention strategies that I looked at:
1. New Zealand: Prescriptions for Exercise
Becoming standard practice in the early 2000s, New Zealand doctors were among the first to begin writing “Green Prescriptions” for physical activity and outdoor time. Patients with conditions like hypertension, diabetes, or anxiety will get prescribed tailored fitness plans, often including subsidized access to gyms or walking groups, instead of jumping right into drug prescriptions. Many countries have endorsed and adopted this program, including Finland, the UK, and even the United States through the Park RX America platform.
According to a New Zealand Public Health Study:
- 42 per cent of patients who stuck to the program permanently increased their activity
- 64 additional minutes per week of exercise were reported by participants
With Canada’s immense parkland across the country it is no surprise that similar “nature prescriptions” already exist in Saskatchewan, Ontario, BC, and Manitoba. Health care providers in those provinces can prescribe time in nature with a Parks Canada Discovery Pass. However, more research is needed to be able to determine if there have been any significant improvements to participants’ health from these programs. But this is definitely a positive start.
Perhaps Canadians might also benefit from being provided with written prescriptions to exercise more frequently.
2. Japan: Waistline Warnings & Forest Therapy
The impressive health of the Japanese population, along with the country’s thriving health care system, are already well-known facts, so it should come as no surprise that two of their practices have made the list.

1. Japan’s “Metabo Law,” implemented in 2008, requires adults aged 40–75 to undergo annual waistline checks at their work. Those who measure over 33.5 inches (men) or 35.4 inches (women) get taxpayer-funded nutritional and exercise counselling provided by the Japanese government.
This might seem a little strange and intrusive to Canadians, but it’s definitely an interesting example of another country taking preventative care seriously.
2. The second example is “Shinrin Yoku” or “forest bathing”. It’s a Japanese program that draws millions into government-certified forest trails to go for walks in nature, promoting stress relief at the same time.
The health benefits of forest therapy include:
- Increases “natural killer” immune cells linked to cancer prevention
- Reduces cortisol levels and blood pressure
- Over 5 million participants per year walk certified trails
3. UK: Traffic Light Labelling on Food
Like many countries, the UK has high rates of obesity– with 63 per cent of adults in England in 2020 being classified as overweight – prompting the government to increase spending significantly in “personalized prevention.” But this isn’t the country’s first run at preventative health.

Since 2006, the UK Department of Health and the Food Standards Agency (FSA) have promoted a system of food marketing, coined “traffic light labelling.” This was implemented as a way to promote healthier eating habits, while disincentivizing poorer ones. Color-coding (red/amber/green) was used to indicate either high, medium, or low levels of total fat, saturated fat, sugar, and salt.
Although ultimately voluntary, this system was adopted by several big-name grocers such as Sainsbury’s, Waitrose, and Co-Op and has inspired the emergence of a similar practice in France. UK Reports show that this type of labeling not only empowered consumers to make healthier choices, but it also encouraged companies to begin making their food healthier– the more red lights your product has, the less likely a consumer is to buy it.
No intrusive government intervention, just a simple voluntary business practice that could enhance consumer knowledge, improve citizens’ eating habits on a large scale, and hopefully encourage companies to make better food.
4. Finland: The Diet That Saved a Province
In the 1970s, Finland’s North Karelia region had the highest heart disease rate in the world. Most people there ate lots of salt and animal fats without many vegetables or fruits. Smoking was also very common. The government wanted things to change, so it came up with a comprehensive plan aimed at radically changing lifestyles. It included organized efforts to change how food is produced, distributed, and consumed, as well as local food campaigns and anti-smoking measures. For instance, it held multiple “Health Day” campaigns in local supermarkets where customers could take a cholesterol test and blood pressure measurement free of charge.
Between 1972-2012, The North Karelia Project was responsible for a massive societal shift:
- Cardiovascular deaths in working-age men dropped by 82 per cent
- Smoking fell from 52 per cent to 33 per cent
- Fat content in meat and salt content in bread dropped
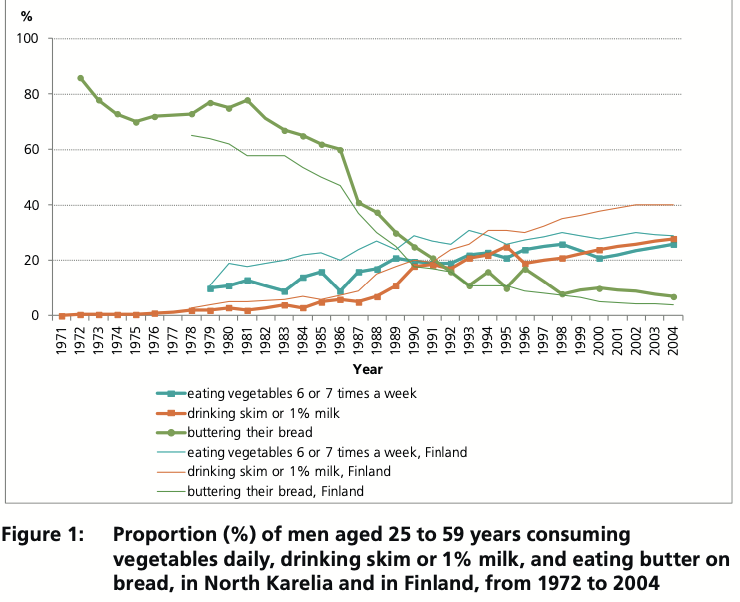
One of the more interesting examples from this project is the testing of cholesterol and blood pressure in grocery stores. This gives patients a voluntary option to check-in and learn about how they can improve their health. So how could Canada learn from this? Bring health information and education to people’s everyday lives.
5. Turkiye: Learn Your Ideal Weight, Live Healthy
Ranking first in all of Europe for rates of overweight and obesity– with almost 67 per cent of the population affected– the Turkish health minister has spearheaded a recent “public weighing campaign.” According to Turkish media, this campaign involves measuring citizens’ height, weight, and Body Mass Index (BMI) in public spaces across all 81 provinces. It’s a voluntary program, so people aren’t required to listen to health care bureaucrats on the street.
Beginning on May 10 this year, those who are assessed as having a BMI of 25 or higher were directed to Healthy Life Centers to receive nutritional counseling from registered dietitians. The health minister himself was even subjected to the scale, and after announcing his BMI was over 25 he joked “which dietitian should I go to?”

This campaign is relatively new so there is no way to accurately gauge its success– and public opinion so far is somewhat negative. What do you think of this campaign? Perhaps Canadians might be more interested in an approach that doesn’t involve weighing people on the street, but instead shares information about diet and exercise that can improve personal health?
So What Should Canada Do?
Without a doubt, Canada needs health reform to improve how our health care system functions and the choices available to patients. The reality is that many health problems are due to aging, genetic conditions and other factors – and so we will never be able to fully “prevent” all demand for health services.
However, if we want shorter wait lists in the health system, we would benefit from having a healthier society in the first place. And for a country like Canada– where people need more care than there is available– we can’t afford to neglect this option.
Although the examples aren’t all perfect fits for Canada, these five countries and their health strategies can act as inspiration for governments in Canada to identify ideas that promote health in creative ways while not limiting citizens’ freedoms.
Jane Gordon served as an intern with SecondStreet.org during the summer of 2025
Share on Facebook
Share on Twitter
You can help us continue to research and tell stories about this issue by making a donation or sharing this content with your friends. Be sure to sign up for our updates too!








