Column
Report
A look at Winnipeg’s city council pension

A little while ago, I did a bit of research into Winnipeg’s City Council pension plan and thought I would post the findings in case anyone would like to take a closer look.
In short, here’s the big picture calculation – over the past 10 years for which data is available (2009-2018), taxpayers and council members contributed the following amounts to the pension:
Taxpayers paid: $4,375,848
Politicians paid: $925,433
In other words, Winnipeg taxpayers put in about $4.73 for every $1.00 put in by members of Winnipeg’s city council. You can see all the data for each year if you – click here.
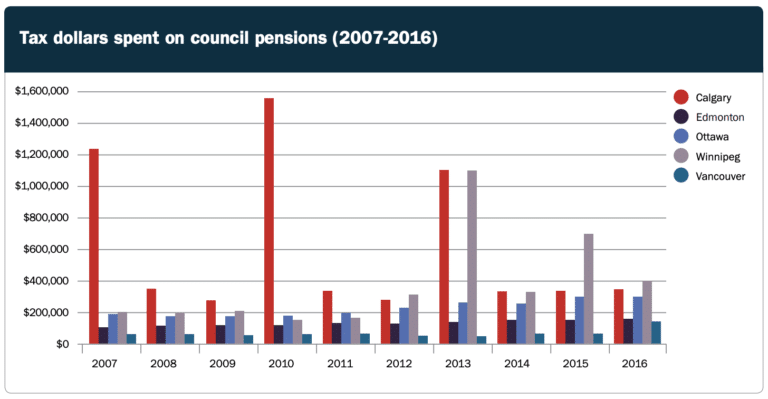
As you can see from this report that I wrote while working for the Canadian Taxpayers Federation, the bill is quite high compared with other cities – Winnipeg taxpayers paid more for their council’s pension than Ottawa and Edmonton combined between 2007-2016.
Winnipeg’s city council has shown it has the appetite for pension reform as of late – they recently attempted to amend the Winnipeg police pension. More recently, the city has also claimed it could be facing a $73 million shortfall if COVID-19 continues until July.
In light of those two factors, perhaps council might want to review its own pension?
In the grand scheme of the city’s budget, the savings would not be significant in a single year. However, as council addresses the city’s cost pressures, it will be hard for them to ask city employees to tighten their belts if council hasn’t tightened its own.
If Winnipeg does decide to review its council pension situation, the City of Edmonton is one worth replicating. As you can see from the bar chart on page 6 of the aforementioned CTF report, Edmonton’s city council pension costs are smooth over time and don’t spike like Winnipeg’s does.
The bill for Edmonton’s council pension doesn’t spike because it’s structurally different from Winnipeg’s – they have what’s known as a “defined contribution” pension as opposed to a “defined benefit” pension. In plain English, their plan protects taxpayers from having to bail out the pension with large sums of money whenever the plan runs into trouble.
Edmonton’s pension may not be as generous as Winnipeg’s, but it’s still better than what 77% of those who work outside of government receive – no workplace pension at all.
Unless Winnipeg fundamentally changes the structure of its council pension plan, taxpayers should expect to pay more and more in the years ahead to continually bail it out. Just wait until there’s an update on the funds in council’s pension in light of the current recession…
Author: Colin Craig


